IVF and the ethics behind it
Srija Sirumalla • 2024-05-06
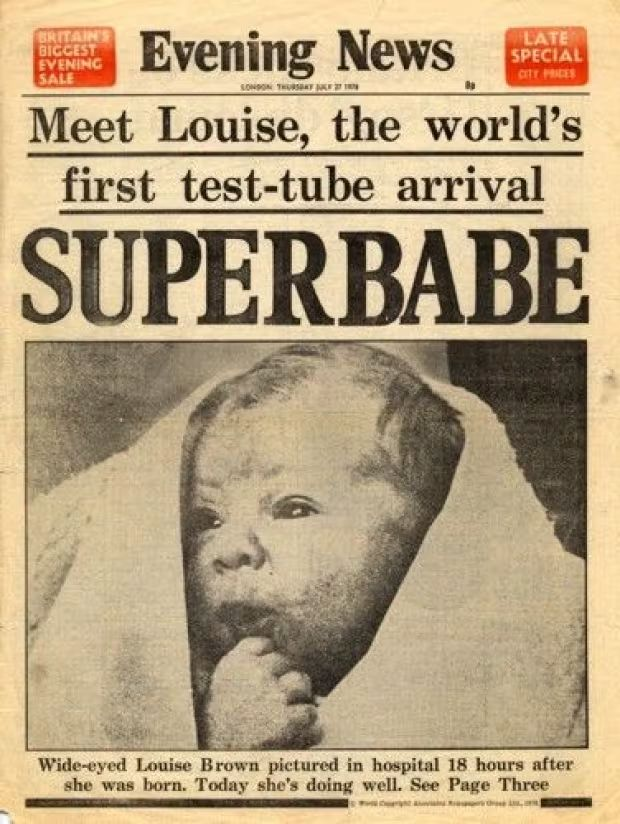
𝙄𝙣𝙨𝙩𝙞𝙩𝙪𝙩𝙚 - 𝙇𝙤𝙣𝙙𝙤𝙣 𝘿𝙚𝙨𝙞𝙜𝙣 𝙖𝙣𝙙 𝙀𝙣𝙜𝙞𝙣𝙚𝙚𝙧𝙞𝙣𝙜 𝙐𝙏𝘾 In Vitro Fertilisation (IVF) has become a widely accepted infertility treatment option for infertile couples to be able to conceive since the birth of Louise Brown on 25th July 1978.
In Vitro Fertilisation (IVF) has become a widely accepted infertility treatment option for infertile couples to be able to conceive since the birth of Louise Brown on 25th July 1978. It is a procedure that is only sought out after the failure of multiple fertility therapies, as it is an expensive to the NHS and emotionally demanding procedure and is conducted by reproductive endocrinologists. In this article, I will be going over the ethical and moral considerations about this treatment.
To be able to discuss the ethics behind this procedure we need to first understand what goes on during the treatment. The NHS guidelines state that “IVF should only be offered to women under the age of 43 who have been trying to get pregnant through unprotected sex for 2 years” So, what happens during IVF?
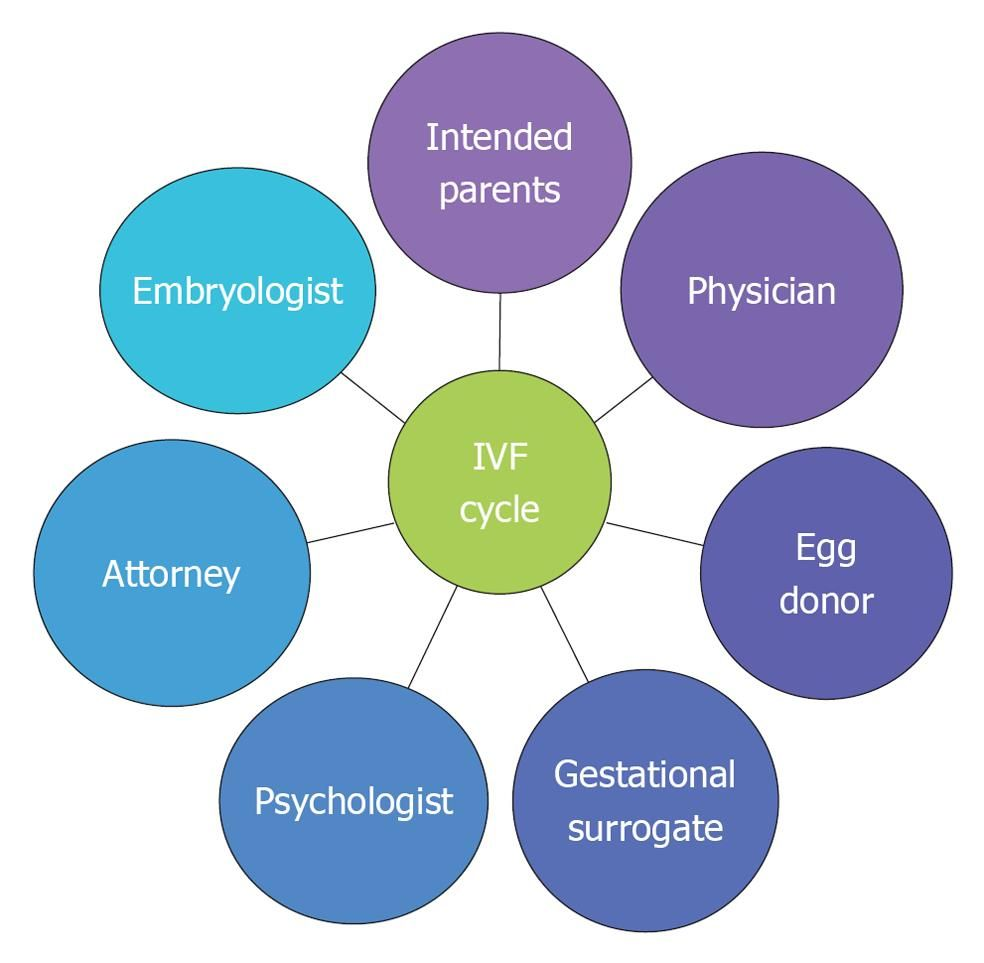
Firstly, the couple goes through several pre-cycle tests to help reproductive endocrinologists identify any factors that may influence the treatment. IVF begins by supressing the would-be mother’s menstrual cycle through medication, in the form of a daily medication or nasal spray which is to be taken over the course of two weeks.
Then the would-be mother is instructed to take a fertility hormone called Follicle Stimulating Hormone (FSH) which is used to encourage the ovaries of the would-be mother to produce more than one egg at a time to ensure that more eggs can be collected and fertilised which gives the reproductive endocrinologist a greater range of embryos to use in the treatment. The clinic providing the treatment would be closely monitoring the would-be mother’s ovaries through vaginal scans. Before the eggs are collected the would-be mother would be given an injection of a hormone called Human Chorionic Gonadotrophin (hCG) which helps the egg cells mature. The would-be mother would be sedated, and the egg cells would be collected using a needle that passes through the vagina and into the ovaries with ultrasound guidance. In some cases, the would-be mother might experience cramps and/or a small amount of vaginal bleeding. The would-be mother will also be given hormone medicines to prepare the lining the womb to be able to receive and house the embryo. Meanwhile the would-be father would be requested to produce a fresh sperm sample after which the sperm are washed and spun at a high speed so only the healthiest sperm could be used for the treatment.
The egg cells collected from the would-be mother will be fused with the wouldbe father’s sperm in a laboratory in order to fertilise them. Although in some cases, the egg cell may need to be injected individually with a single sperm in a process called Intra Cytoplasmic Sperm Injection (ICSI). The fertilised embryos will continue to be grown in the laboratory for up to six days before being transferred into the would-be mother’s womb. The embryos are then transferred into the womb using a thin tube called a catheter that is passed into the would-be mother’s vagina and the number of embryos that will be transferred must be discussed beforehand with the would-be parents.
Now, moving onto discussing the ethics. The ethical arguments started when the first research reports and articles on animal IVF experiments were first published in the mid 1930s. Although some people saw it as promising technology to help those struggling with infertility some saw it as blasphemy against God and these negative perceptions towards IVF only grew with the birth of the first human child Louise Brown in 1978 and the protests grew even stronger when scientists attempted to introduce IVF to America and the rest of the world.
Firstly, we need to understand that the chance of having a healthy baby after IVF is 48% for women under 30 and this probability decreases as the would-be mother gets older. In some cases, it may result in an ectopic pregnancy (when a fertilised egg implants itself outside of the womb, usually in the fallopian tubes.). Ectopic pregnancies can be life threatening if the fertilised egg continues to grow in the fallopian tubes which causes the fallopian tubes to rupture, which then causes severe bleeding, infection and sometimes even death, but the chance of an ectopic pregnancy is between 1.4% to 8.6%. When it comes to bioethics, the facts and values are considered, but religions rely solely upon the values and scriptural beliefs. It’s hard to conclude what each religion’s views on IVF are as there are multiple denominations which have different beliefs and interpretations. In 2007 Pope Benedict XVI declared IVF and other methods of assisted reproduction invalid as some embryos (considered the beginning of life by many) are discarded and because these treatments go against the principle of marital sex which according to Christian beliefs unite the couple. In protestant countries however, IVF is no longer disputed but the Church of England has expressed concern regarding IVF treatment being offered to single women and same sex couples. The failure of being able to conceive an offspring would lead the couple to have emotional difficulties such as guilt, anger, disbelief and grief over the loss of an imagined child, personal life goals, an expected lifestyle and perhaps even a recognised status in society, as in some cultures having a baby is believed to “kick-start” the marriage.
Additionally, failing to conceive for the nth time would shatter the confidence of the would-be mother and send the would-be mother down a spiral of an identity crisis.
The failure of IVF could place a burden on the couple’s relationship, finances (if they opted for a treatment with a private infertility clinic) and careers. It could lead the individuals to isolate themselves from their family and friends due to the fear of being judged or even embarrassment, paired with the social pressure to recover and lack of emotional support will affect the couple’s capacity to grieve which would have an extremely negative impact on the couple’s mental health. Researchers have found that around 40% of fertility patients had experienced suicidal feelings and that 10% have experienced suicidal feelings quite often or all the time.
20% of infertility patients tend to experience increased levels of anxiety and depression. It is important to note that the injections of hormones cause pain, discomfort and anxiety peaks and troughs.
Lastly, couples end up paying lavish amounts of money for their own treatment as some hospitals don’t offer it for free, which has a low chance of conceiving and may result in emotional difficulties. I feel that for a country that pioneered IVF, the NHS and us as a society need to do more to support those facing emotional difficulty before, during and post IVF treatments.
References links -
https://www.nhs.uk/conditions/ivf/
https://www.bbc.co.uk/news/uk-england-cambridgeshire-65646682
See More Posts
Copyright © 2021 Govest, Inc. All rights reserved.